As the COVID-19 pandemic began to spread worldwide in the early part of this year, one of the first things to become clear was the supply of personal protective equipment (PPE) – facemasks in particular – was not ready for the ensuing surge in demand. In many parts of the world impacted by the coronavirus, facemasks were not commonly worn, and N95 was not a concept with which people were generally familiar.
Much has changed since then, and while there are certain countries where the use of facemasks and the understanding of their capabilities is still very much in the learning-curve phase, the demand has gone from select workplace environments to a scenario where a large portion of the global population is seeking facemasks for everyday use. This has stressed the supply chain for a variety of reasons, but it has also put significant pressure on the organizations who are involved in testing and validating the performance of various types of facemasks – from N95 respirators (and their equivalents worldwide) to surgical facemasks and others.
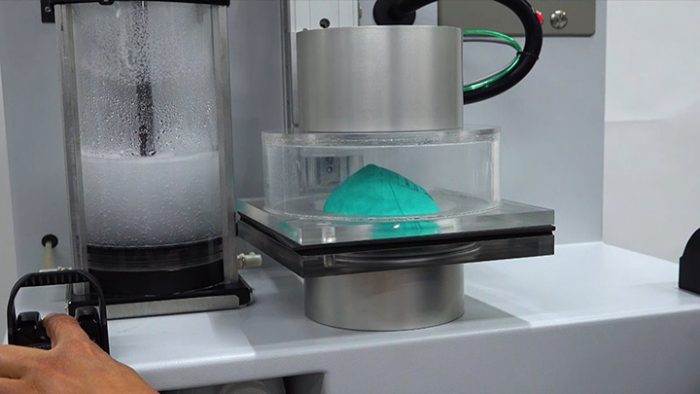
Air Techniques International, a designer and manufacturer of specialized testing equipment for HEPA filters, media, filter cartridges, respirators and protective masks based in Owings Mills, Maryland, has surged its capacity significantly and is running double shifts since the COVID-19 pandemic took hold. And while ATI’s 100X testing equipment has traditionally been employed for oil-based filter media, Gautam Patel, ATI’s global product manager, says the company is increasingly receiving requests from filter media material suppliers and facemask manufacturers seeking its technology to facilitate the aerosolized sodium chloride testing required by the U.S. National Institute for Occupational Safety and Health (NIOSH) to validate the performance of facemasks and the materials that go into them.
Framing the facemask landscape
Facemasks are employed in a variety of different applications, such as construction, industrial, medical, etc. For the purposes of this article, we will focus on medical applications, as these are the mask types that have been under the spotlight during the COVID-19 pandemic.
“The NIOSH standard for facemasks is a standard with ‘teeth,’” says Lindblom. “If a manufacturer doesn’t meet the standard they run the risk of getting their approval rejected by NIOSH. As the filter media is the most crucial part in meeting the efficiency standard, we as a media manufacturer need to make sure that all our products meet the standard.”
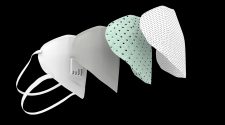
For medical applications, masks can be categorized as surgical or respirator types. For the most part, surgical masks are worn to prevent particles coming out of the mouth or nose of the wearer from coming in contact with others. Respirators on the other hand are a tight fit and are used to protect the wearer from harmful particles coming in contact with them.
From a supply chain perspective, the material required for respirator-type facemasks, commonly known as meltblown, has been a key stumbling block. “The supply situation is still an ongoing challenge. The demand is unprecedented and will continue to be so for the foreseeable future,” says Per Lindblom, global segment leader for Hollingsworth & Vose’s Respiratory Protection business. “It is relatively easy to add facemask capacity versus adding meltblown capacity due to the complexity of the machines and costs. The increase of mask capacity has so far exceeded the increase of meltblown.”
Meltblown is the ideal material for respirator-type facemasks because it offers high filtration efficiency, with excellent breathability. “Breathability is an important factor to consider,” says Todd Hillam, a senior scientist with Nelson Labs. “Although there may be plenty of materials out there that can offer a high level of filtration efficiency, not all of them are breathable, and if you can’t breathe through them, or they require bypass to breathe, then the material isn’t filtering and they may not be safe to use and will not meet N95 respirator requirements.”
In the U.S., the Centers for Disease Control (CDC), Food and Drug Administration (FDA), and NIOSH – a unit of CDC – are involved in the regulation and validation of surgical and respirator masks. In Europe, the European Committee for Standardization (CEN) is responsible for the regulation of masks. And in China, surgical and respirator masks fall under the jurisdiction of the Standardization Administration of China. Medical applications are part of the National Mandatory Standard Program, meaning the standard requirements must be met for masks to be approved for use.
Surgical-type masks
For surgical masks in the U.S., there are five different tests the FDA recognizes that are found in the ASTM F2100 standard – bacterial filtration efficiency (BFE), differential pressure, sub-micron particle filtration efficiency (PFE), synthetic blood penetration and flammability. Based on the performance of the facemask material manufacturers can classify as Level 1-3.
In Europe, surgical masks fall within the scope of the EU legal framework on medical devices – Council Directive 93/42/EEC, which will be replaced by Regulation (EU) 2017/745 in May 2021. Under the EU regulation, surgical masks must be designed, manufactured and tested according to the methods specified in EN 14683 + AC (2019) to demonstrate compliance with performance requirements in terms of bacterial filtration efficiency (BFE), breathability, splash resistance and microbial cleanliness.
In China, there are two standards for non-respirator facemasks employed in medical settings – YY/T 0969 and YY 0469. YY/T 0969 is designed for masks used in the general medical environment, while YY 0469 is designed for masks worn by medical staff during a medical procedure, such as an operation. Both standards establish requirements for test methods, marking, instructions for use, packaging, transport and storage.

Respirator-type masks
For N Series respirators (N95, N99, N100) and their equivalents in Europe (FFP2, FFP3) and China (KN90, KN95, KN100), different regulations and standards apply. In the United States, the federal regulation for certifying air-purifying particulate respirators is 42 CFR Part 84. Testing follows the procedures outlined by NIOSH based on the guidelines set forth in 42 CFR Part 84.
In Europe, respirators are considered PPE and fall under the scope of Regulation (EU) 2016/425. EN 149:2001 is the standard, which specifies the minimum requirements for filtering half masks used as respiratory protective devices, specifically against particles, and the required laboratory and practical performance tests to assess mask compliance.
In China, KN95s are regulated by the Chinese government through the Standardization Administration of China. The applicable standard is GB 2626, which was recently updated. The effective date of the updated GB 2626-2019 was postponed from July 1, 2020 to July 1, 2021 to ensure a stable supply as China continues to respond to the COVID-19 pandemic. GB 2626 specifies technical requirements for respiratory protection, including appearance check, filter efficiency, inward leakage performance, respiratory resistance, exhalation valve, dead space, visual field, head harness, connection and connecting parts, lens, air tightness, flammability, cleaning and disinfection, practical performance, information provided by the manufacturer, and packaging.
The testing process
The testing of facemasks and their materials of construction is multi-faceted. For material suppliers, testing is not required, but it is often performed to provide the facemask manufacturer a sense of security when sourcing materials for the masks they produce.
In the U.S., N Series masks like the N95 are tested using samples from lots or batches, and the test itself is destructive, so the cost of having material that does not meet the standard requirements is significant. As such, reputable material manufacturers test their filter media before they even send it to the facemask manufacturer.
“N95 masks need to comply with the NIOSH 42 CFR Part 84 Respiratory Protective Devices standard. We derive the testing of the filter media from this standard to make sure that our customers pass the standard without any problems,” says Lindblom. “This means a mask made with H&V media will have an efficiency that far exceeds the 95% efficiency [required by the standard], while providing low resistance.”
At the facemask manufacturer level, the stakes are higher, as the mask manufacturers are interfacing with the regulatory agencies themselves. In the U.S., that is NIOSH, with the FDA overseeing medical applications.
“The NIOSH standard for facemasks is a standard with ‘teeth,’” says Lindblom. “If a manufacturer doesn’t meet the standard they run the risk of getting their approval rejected by NIOSH. As the filter media is the most crucial part in meeting the efficiency standard, we as a media manufacturer need to make sure that all our products meet the standard.”
“The mask manufacturer must ensure the product meets the requirements of 42 CFR Part 84 before they can go to NIOSH,” says Hillam. “Precertification testing is performed by an approved third-party lab like Nelson Labs. Samples can then be submitted by the mask manufacturer to NIOSH for further testing and review.” For N Series respirators, NIOSH also conducts a fit test.
For N95 respirators used in medical applications, the FDA requires additional testing to show protection for fluid resistance, flammability and biocompatibility.
In addition to its testing regime, NIOSH has a quality control program, which includes inspection of the manufacturing plant and random testing of certified masks in the marketplace to ensure ongoing compliance. For surgical masks and respirators to be used in medical applications, the U.S. also requires FDA clearance. Although, the FDA has made some concessions to streamline the clearance of masks and respirators during the COVID-19 pandemic.
In Europe and China, the testing requirements for surgical masks and respirators are similar to the U.S., with some slight differences. For example, the standard testing procedures in the U.S. require fluid resistance testing at all three levels for surgical masks, while Europe requires fluid resistance only for Type IIR surgical masks. Europe requires a test for microbial cleanliness, while the U.S. does not.
Extreme circumstances
As the COVID-19 pandemic began to spread worldwide and the supply of surgical and respirator-type facemasks became stressed, governments responded by, in select cases, loosening and/or streamlining their requirements for facemasks to enter the market.
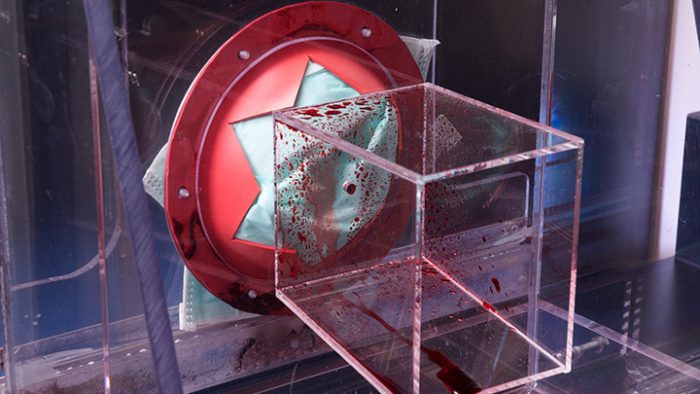
For example, on Feb. 4, 2020, the U.S. Health and Human Services Secretary, Alex Azar, declared that “circumstances exist to justify the authorization of emergency use of additional respiratory protective devices in healthcare settings during the COVID-19 outbreak.” As such, the FDA issued Emergency Use Authorizations (EUA) for respirators and other types of personal protective equipment. These EUAs authorized all NIOSH-approved particulate-filtering air purifying respirators (APRs) to be used in healthcare settings, including all NIOSH-approved filtering facepiece respirators, elastomeric APRs, powered APRs, expired NIOSH-approved filtering facepiece respirators, and respirators that had been decontaminated pursuant to the terms and conditions of an authorized decontamination system. In addition, certain non-NIOSH-approved disposable filtering facepiece respirators were permitted for use.
According to Hillam, the FDA’s EUAs have made for a quicker, more streamlined testing process. “The testing requirements have become somewhat less involved due to the emergency use with an abbreviated clearance process,” he says. And while the FDA has truncated its process somewhat, NIOSH has not. As such, Hillam says Nelson Labs is recommending that its customers use their NIOSH precertification data for FDA approval to start using their respirator mask while at the same time applying for NIOSH certification.
It is also important to note that even though a manufacturer has completed an abbreviated testing protocol to get their device released under the EUA, this does not mean that the device is FDA cleared. The EUA policy is intended to remain in effect only for the duration of the public health emergency related to COVID-19. The manufacturer will need to complete the full battery of testing required if they would like to keep their product on the market after the EUA has been withdrawn.
While the FDA’s EUAs were designed to help free up additional supplies of much-needed surgical and respirator facemasks, as well as other PPE and medical supplies, they haven’t been executed without flaw. In early June, the FDA rolled back its EUA for the decontamination of certain types of respirators due to concerns about variances in the design and design features, such as exhalation valves, which may not support effective decontamination. The FDA also was forced to roll back its EUA on non-NIOSH-approved respirators manufactured in China when NIOSH tests showed some of the approved respirators from China had failed to demonstrate a minimum particulate filtration efficiency of 95%.
In China, the rush to get surgical masks and respirators to market has caused significant quality control issues. Masks, other forms of PPE and testing kits coming from China have, in some cases, failed to meet minimum requirements in Europe and the U.S., raising concerns about counterfeit and/or poor manufacturing practices.
In response, the Chinese government implemented a program to inspect every shipment of respirators, ventilators and other medical supplies for quality issues before export. As part of this program, the Chinese government requires companies exporting medical facemasks that have obtained certification or authorization from other countries to submit a declaration in writing together with customs declarations, as a warranty of compliance with the standards and safety requirements of the importing countries.
“Because there are so many new players, the demand is so high and the production has ticked up so much, there are a lot of new products and designs that may not meet all the performance requirements in the standards,” says Hillam. As such, he says it is important for buyers, particularly in medical scenarios, to look beyond the labeling claims on the masks they buy and seek out concrete data to support the performance specifications. Hillam also recommends that buyers reference NIOSH’s list of approved manufacturers, located on the NIOSH website, whenever working with a new respirator manufacturer.

The road ahead
One of the challenges in getting surgical and respirator facemasks into the hands of the medical community during the COVID-19 pandemic has been the lengthy testing process required to validate the performance of different mask types. And while there have been efforts made to streamline the process, such as the U.S. FDA’s Emergency Use Authorizations, those efforts have stumbled at times.
Perhaps one of the lessons to be learned from COVID-19 will be the need for an emergency response strategy for streamlining testing requirements to enable the supply to ramp up more quickly, and safely, in times of tremendous need.
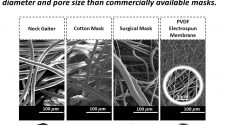
Likewise, as the general public has become more familiar with different types of facemasks, there will likely be innovation in the area of facemask materials and facemask design. Some areas prime for innovation include the development of mask materials that are reusable while maintaining a high level of performance, as well as meltblown alternatives for facemask filtration media – both of which would help expand the potential supply of facemasks going forward.
In considering the supply chain challenges the global facemask market has faced during the COVID-19 pandemic, one of the clear takeaways is there isn’t enough material to be had to support a scenario where the bulk of the global population is seeking facemasks for everyday use. As such, Hillam says he expects to see innovation on the material front. Likewise, he says there is a need for standards to evolve to support general-use applications, which has already started in the ASTM International standards committees.
For example, there is some discussion in the material science and standards communities in the U.S. to develop a new specification for respirator-type facemasks for the general public, à la an N80 respirator. This would enable more material types to be employed in respirator-type facemasks, thus increasing the potential supply significantly, while also offering a mask option that would provide a strong level of protection for the public at large.