People spend 90% of their time in indoor environments, making air quality one of the most profound health implications for the world’s population. Addressing this global public health concern requires a clear understanding of the transmission processes of infections by developing and implementing targeted infection prevention and control measures.
Worldwide outbreaks of severe acute respiratory syndrome (SARS) and other viral agents have caused a substantial health impact on the population and have increased public concerns about the spread of viral disease. The global pandemic caused by the novel coronavirus SARS-CoV-2, which caused the disease known as COVID-19, has changed the world in ways no one could have imagined. There is much more to learn about this ever-changing global threat. However, some aspects of the virus are known, such as its main route of transmission being that of an airborne nature. Therefore, there is a strong effort to mitigate risk to the general population through the use of engineering controls such as improved air filtration.
A Word on Particles
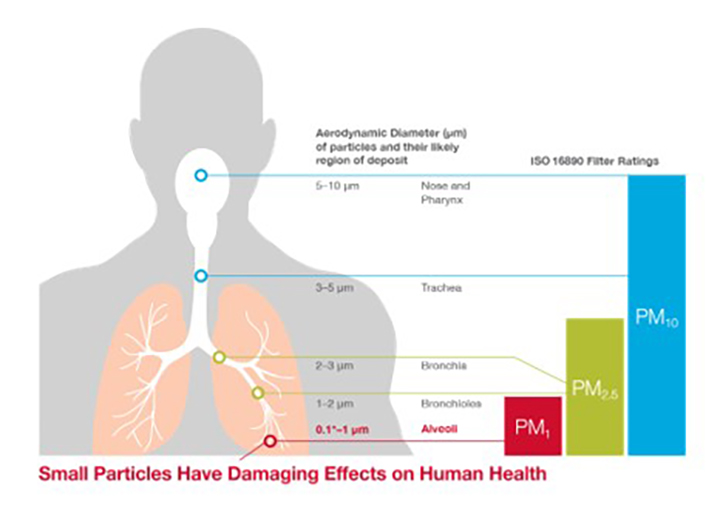
As it relates to human health, particles with a diameter of 10 microns or less (≤ PM10) can penetrate and lodge inside the lungs. Particles with a diameter of 2.5 microns or less (PM2.5) can penetrate deeply into the lungs, particles less than 0.5 microns in size can pass through the blood/gas barrier and enter the bloodstream, and chronic exposure to particles contributes to the risk of developing cardiovascular and respiratory diseases, as well as lung cancer.
Particles can be viable or non-viable in nature. Viable particles contain one or more living organisms such as bacteria or fungi, and their size generally ranges from 0.2-30 microns. Viable particles can survive and replicate independently. Non-viable particles include particles that commonly consist of a complex mixture of solid and liquid particles of organic and inorganic substances suspended in air. Viruses are in a different classification, in that they are parasitic, not free-living or able to transport themselves, and require a transport particle followed by a host to survive and replicate. Non-viable particles are the main source of movement for all other particles and are commonly referred to as transport particles.
Background on Viral Testing at AAF Clean AIR Center
In 2015, the University of Minnesota developed a test to evaluate filter performance using a 50-nanometer swine virus, an adaptation of the ASHRAE 52.2 (2012) method, and molecular virology to quantify the percent reduction of virus with mechanical capture based on transport particles entrapped within filter media. The goal of this study was to develop a standardized method to evaluate filter performance against a virus of interest in the swine industry and ultimately provide producers with a procedure to evaluate filter efficiency.

In 2018, before the coronavirus pandemic, AAF Flanders worked with the University of Minnesota to replicate this academic test and apply it to industry. This test was fully replicated and implemented in AAF Clean AIR Center’s Biological Laboratory as a first in the air filtration industry-test capability. Testing was originally done on viruses endemic to pigs, similar to that of the University of Minnesota, due to a growing concern for virus spread and an increase in filtration in animal husbandry.
The test is conducted using a modified ASHRAE 52.2 standard method, where a standardized ASHRAE test duct is utilized, and filters of different efficiencies are challenged with an aerosolized solution of potassium chloride (KCL) particles tagged with a fluorescent dye and the virus of interest in vaccine form. The system operates between 650-1968 cfm, depending on the industry under evaluation, and aerosols were generated using a high-volume aerosol generator.
Air samples were collected upstream and downstream of the filter using Anderson Cascade Impactors with sizes ranging from 0.3-10 um. Virus particles, KCl, and fluorescent tracer dye are physically captured on impactor plates, and the virus is subsequently removed and purified to quantify using reverse transcription polymerase chain reaction (RT-PCR) and a fluorometer to estimate the mass of the particles. For each particle size, the removal efficiency was calculated1 (National Hog Farmer, 2015).
The results at both the University of Minnesota and AAF were reproducible and proved, that under the conditions of the study, filter efficiency for a virus was similar to the ASHRAE 52.2 tested efficiency of a filter2 (Schulz, 2019).
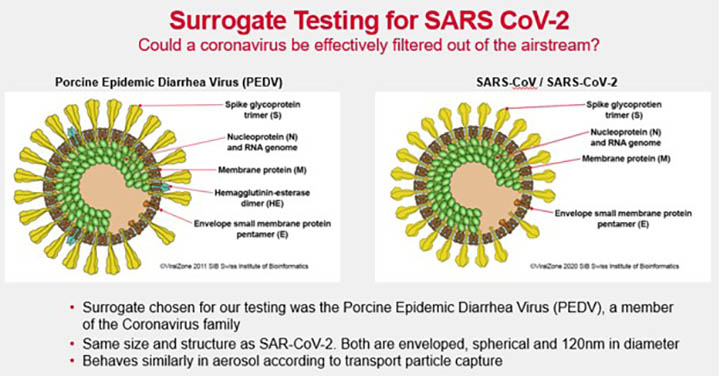
At the beginning of the pandemic, the question was posed “Could a member of the coronavirus family also be filtered out of the airstream?” AAF Clean AIR Center scientists and engineers drew on previous research to quickly develop a test plan using a safe surrogate virus with properties similar to those of SARS-CoV-2. For this study, the Porcine Epidemic Diarrhea virus (PEDV) was chosen since it is the same 120-nanometer size and spherical structure and behaves similarly in aerosol according to transport particle capture.
The Clean AIR Center’s Biological Research Department launched a study utilizing a safe surrogate for the SARS-CoV-2 virus to evaluate the virus removal efficiency of several filters ranging in efficiency ratings from MERV 14 to HEPA. Filters were challenged with a solution of 10% KCl, PEDV-killed adjuvanted vaccine with a virus concentration of 10⁸ viral RNA copies/ml, 0.03% fluorescein tracer dye for particle mass, a flow rate of 2000 cfm, and temperature and humidity controlled according to the ASHRAE 52.2 test standard.
Air samples containing surrogate viruses were collected upstream and downstream from the filters using aerosol test equipment such as Anderson Cascade Impactors and optical particle counters to be able to separate particles by size (approximately 0.3 to 10 microns). The samples were then quantified by reverse transcription polymerase chain reaction (RT-PCR) and a fluorometer to estimate particle mass. For each particle, the particle size removal efficiency was calculated.
The results showed that under the conditions of the study, filter efficiency for SARS-CoV-2 surrogate and other viruses was comparable to filter efficiency using KCl particles (ASHRAE 52.2 standards). In addition, the efficiency of particle removal was similar across the methods used (optical particle counter, fluorometer, or PCR).
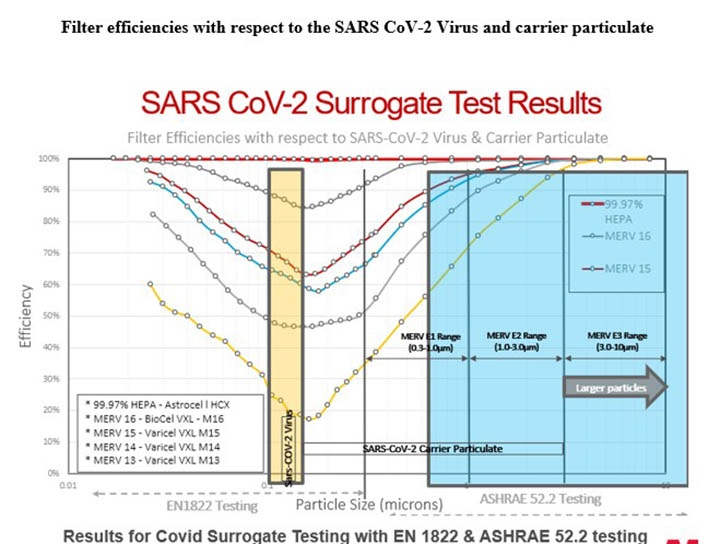
Results for COVID Surrogate Testing with the ASHRAE 52.2 test method showed that for each air filter tested, virus capture is not independent of particle removal efficiency. The percentage of airborne coronavirus-carrying particles was reduced with an increase in MERV rating. This was the first industry result of this type which was significant to substantiate the pandemic mitigation strategy of targeting bioaerosols with engineering controls, such as filtration. Air filtration does provide the removal of viral particles in aerosol and can help mitigate the spread of airborne viruses, with the caveat being that the aerosol must enter the air handling system for it to be effective.
In addition to the ASHRAE 52.2 test method adaptation, AAF also tested filters against particles smaller than 0.3 microns using the EN1822 test methodology. It was determined that filtration efficiency for all types of filters is lowest from around 0.1-0.2 microns, called the most penetrating particle size or MPPS, and increases again as particles become smaller.
As can be seen in the graphical representation, high MERV-rated filters will reduce airborne viruses. Even though viruses are much smaller than 0.3 microns, filters that can remove particles under 1 micron will also effectively remove viruses. HEPA filters are the best way to eliminate possible contamination, but where HEPA filters can’t be used, upgrading to the highest MERV filter available will offer the best protection.
Filter Efficiencies with Respect to the SARS CoV-2 Virus and Carrier Particulate
In conclusion, the results of these studies have consistently shown that airborne microorganism capture is not independent of filter efficiency. Filters are an effective tool for removing any type of airborne microorganism, assuming the particles enter the air handling system. If a filter can remove a non-viable transport particle, it will also remove a viable particle of the same size. Implementing higher MERV-rated filters as an engineering control can effectively reduce the spread of airborne viruses, such as the Coronavirus.
References:
- Schulz, K. (2019, May 6). Filtering efficiency. National Hog Farmer. https://www.nationalhogfarmer.com/hog-health/filtering-efficiency
- Standards of filter testing for PRRS virus.
National Hog Farmer. (2015, January 12). https://www.nationalhogfarmer.com/market-news/standards-of-filter-testing-for-prrs-virus.





![Figure 1: Heat Exchanger Proventics GMBH.[22]](https://www.filtnews.com/wp-content/uploads/IFN_2_2024_crimpedmicrofiberyarns_Fig.-1-Heat-exchanger-225x125.jpg)